Trauma and PTSD
What Are Trauma and PTSD?
- Trauma refers to the emotional and psychological response to a deeply distressing or disturbing event, such as violence, accidents, or natural disasters. Trauma can leave lasting effects, both mentally and physically.
- Post-Traumatic Stress Disorder (PTSD), on the other hand, is a mental health condition that develops after experiencing or witnessing a traumatic event. While many people experience trauma, not everyone develops PTSD. PTSD is marked by a pattern of symptoms that persist for more than a month after the event and significantly impact daily functioning.
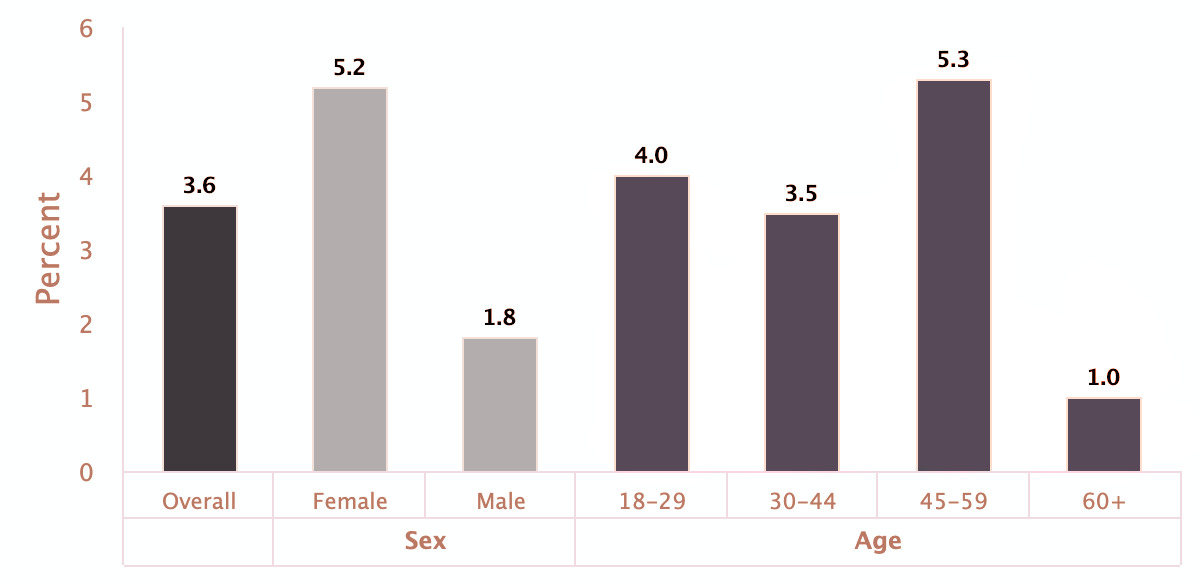
Statistics on PTSD
PTSD affects millions worldwide. According to the National Center for PTSD, about 6% of the U.S. population will have PTSD at some point in their lives, and 12 million adults in the U.S. suffer from it each year. The disorder is more common in women than in men, with women being twice as likely to develop PTSD. In specific populations, such as military veterans, the rates are even higher; studies suggest that up to 30% of veterans develop PTSD after combat exposure.
Prevalence of Post-Traumatic Stress Disorder Among Adults
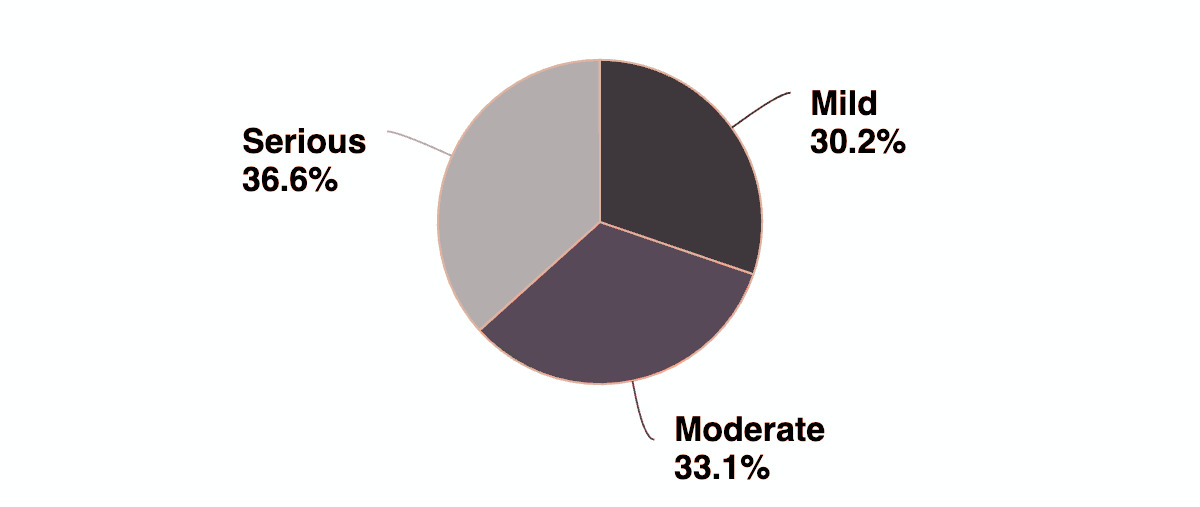
Severity of Post-Traumatic Stress Disorder Among U.S. Adults
 Reference: The charts are from the National Institute of Mental Health (NIMH).
Reference: The charts are from the National Institute of Mental Health (NIMH).
How Clients Present to Therapy with PTSD
Individuals with PTSD often come to therapy displaying a range of emotional, cognitive, and physical symptoms. Some common symptoms include:
- Intrusive memories: Recurrent, involuntary memories of the traumatic event, flashbacks, or nightmares.
- Avoidance: Steering clear of reminders of the trauma, including people, places, or conversations associated with the event.
- Negative changes in mood: Feelings of hopelessness, detachment, emotional numbness, or difficulty experiencing positive emotions.
- Hyperarousal: Being easily startled, feeling tense or on edge, having difficulty sleeping, and experiencing irritability or angry outbursts.
- Episodic amnesia: Difficulty remembering key aspects of the traumatic event, which can leave gaps in the memory.
- Depersonalization and derealization: Feeling detached from oneself or one's surroundings, as if the world isn’t real or you’re living outside of your own body.
Differentiating Diagnosis: When PTSD Masks Other Conditions
Many clients with PTSD initially seek therapy for other presenting concerns, such as depression, anxiety, substance use disorders, or even dissociative identity disorder (DID). In such cases, the underlying cause may be trauma-related, with PTSD being the root issue. Depression, for instance, is a common comorbidity in individuals with PTSD, often leading to feelings of hopelessness or worthlessness. Additionally, substance use disorders may develop as a means of self-medication to alleviate the distress of PTSD. Proper diagnosis is essential to provide targeted treatment.
The Impact of PTSD on Physical and Mental Health
PTSD can take a significant toll on both physical and mental health. Chronic stress and hyperarousal increase the risk of physical conditions like hypertension, heart disease, and digestive issues. Episodic amnesia, a less common symptom, may cause individuals to forget parts of the traumatic event, leading to disorientation and confusion. Mental health symptoms, such as severe anxiety, depression, and suicidal ideation, may intensify without proper intervention.
How PTSD Affects Relationships
PTSD can strain personal and social relationships. Those with PTSD may become withdrawn, avoid social interactions, or experience intense irritability, leading to conflicts with loved ones. A person with PTSD may also feel emotionally numb, making it difficult to engage meaningfully in relationships, further isolating them from support systems. Partners, family members, and friends may struggle to understand the emotional volatility or detachment that can accompany PTSD, which can lead to breakdowns in communication and empathy.
Etiology of PTSD: Why Do Some Develop PTSD and Others Don’t?
While traumatic events are the trigger for PTSD, not everyone exposed to trauma will develop the disorder. Several factors contribute to whether someone is more likely to develop PTSD, including:
- Genetics: Studies have shown that individuals with a family history of anxiety or mood disorders may be more susceptible to PTSD.
- Pre-existing mental health conditions: Individuals with existing mental health issues like depression or anxiety are at higher risk.
- Coping strategies: People with less effective coping mechanisms or limited emotional support are more vulnerable.
- Social support: A lack of strong social support can increase vulnerability to PTSD. Individuals who feel isolated or without a reliable support network may find it more difficult to process traumatic experiences, increasing the likelihood of developing PTSD.
The Importance of Treatment for PTSD
Treatment for PTSD is crucial to improving quality of life and reducing the disorder's long-term impacts on mental and physical health. Without treatment, PTSD can become chronic, leading to ongoing distress and dysfunction in daily life.
Treatment Options for PTSD
- Psychotherapy: Psychotherapy, particularly trauma-focused therapy, is the cornerstone of PTSD treatment. It is highly effective in helping individuals process traumatic memories and reduce symptoms.
- Medications: Antidepressants, particularly SSRIs and SNRIs, are often prescribed to help manage the emotional symptoms of PTSD, such as anxiety and depression. In some cases, medications like prazosin may be used to alleviate nightmares and sleep disturbances associated with PTSD.
- Group Therapy: Group therapy offers the opportunity to connect with others who have had similar experiences, providing support, reducing isolation, and helping individuals gain new perspectives on their trauma.
- Mindfulness and Stress Reduction: Incorporating relaxation techniques, mindfulness, and stress-reduction strategies can complement other therapies, helping clients manage hyperarousal and anxiety symptoms.
How I Can Help
In my years of practice, I’ve worked with individuals who’ve faced deep trauma, including military veterans, survivors of rape, child abuse, and domestic violence. I understand how heavy these experiences can feel, and my focus is on creating a space where you can feel supported and safe as we begin to process them. We’ll move at a pace that works for you, working together to help you regain control and manage the symptoms of PTSD. Using proven, evidence-based methods, my aim is to help you find relief and rebuild your strength, so you can move forward with confidence and a sense of peace.
What you think, you become. What you feel, you attract. What you imagine, you create.
- Buddha, Interpreted from various Buddhist teachings
Reach Out