Depression
Understanding Depressive Disorders
Depressive disorders encompass a range of mental health conditions characterized by persistent feelings of sadness, hopelessness, and a lack of interest in daily activities. These disorders can severely impact an individual's quality of life, affecting relationships, work, and overall well-being. Let’s explore the different types of depressive disorders, along with their symptoms, causes, and the importance of treatment.
Prevalence and Statistics
Depressive disorders are among the most common mental health conditions worldwide. According to the World Health Organization (WHO), more than 264 million people globally experience depression. In the U.S., the National Institute of Mental Health (NIMH) estimates that 7.8% of adults experienced at least one major depressive episode in 2019. Depression is more prevalent in women than men and can occur at any age, with higher rates observed in individuals aged 18 to 25.
Prevalence of Major Depressive Episodes Among Adults:
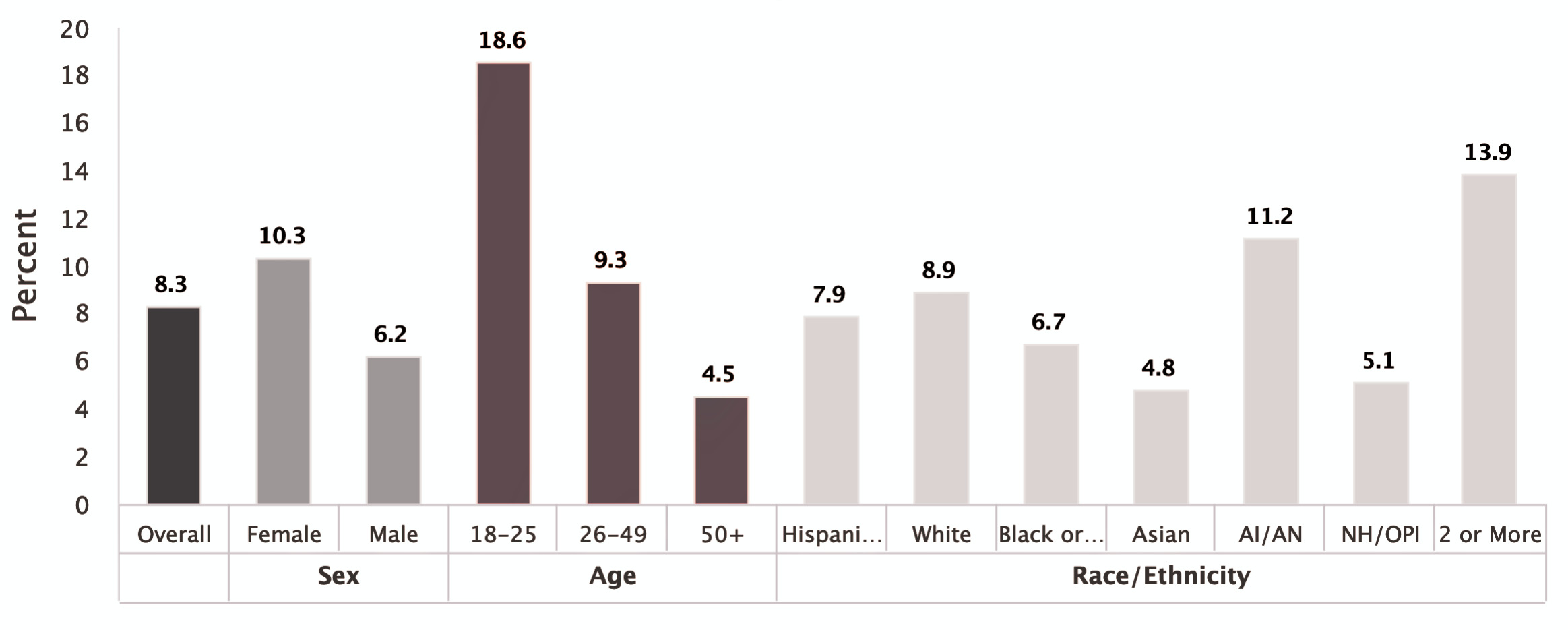 *Persons of Hispanic origin may be of any race; all other racial/ethnic groups are non-Hispanic |
AI/AN = American Indian / Alaskan Native | NH/OPI = Native Hawaiian / Other Pacific Islander.
Reference: The charts are from the National Institute of Mental Health (NIMH).
*Persons of Hispanic origin may be of any race; all other racial/ethnic groups are non-Hispanic |
AI/AN = American Indian / Alaskan Native | NH/OPI = Native Hawaiian / Other Pacific Islander.
Reference: The charts are from the National Institute of Mental Health (NIMH).
Depression in New York City
Urban living in major cities like New York City presents significant mental health challenges. Studies indicate that city dwellers experience a higher prevalence of depression compared to those in smaller cities or rural areas. According to the World Economic Forum, living in a city like NYC increases the risk of depression by 20%.
Major Depressive Disorder (MDD):
Single Episode and Recurrent Types
Major Depressive Disorder is characterized by persistent sadness, hopelessness, and a lack of interest in activities that once brought pleasure. MDD can be categorized into:
- Single Episode MDD: A single period of major depression lasting at least two weeks, often longer. Symptoms may include feeling sad or 'empty,' loss of interest in favorite activities, changes in appetite or sleep (whether increased or decreased), reduced self-confidence and self-esteem, fatigue, difficulty concentrating, feelings of hopelessness, irritability, anxiety, guilt, thoughts of death or suicide, and physical symptoms such as aches, pains, headaches, and digestive problems.
- Recurrent MDD: Individuals experience multiple episodes of depression, with periods of remission in between. The severity of each episode may vary, but without treatment, these episodes can worsen over time, leading to greater impairment.
Dysthymia (Persistent Depressive Disorder)
Dysthymia, also known as Persistent Depressive Disorder (PDD), is a chronic form of depression where individuals experience long-term, low-grade depressive symptoms for at least two years. Although the symptoms of dysthymia may not be as intense as those in MDD, they persist and interfere with daily life. Common symptoms include low energy, feelings of inadequacy, and difficulty making decisions. Because the symptoms are often milder, individuals with dysthymia may go undiagnosed for years.
Other Forms of Depression
- Adjustment Disorder with Depressed Mood: This type of depression occurs in response to a significant life event or stressor, such as the loss of a loved one or a major life change. Symptoms are similar to those of MDD but are directly linked to the stressful event and tend to improve once the individual adapts to the new circumstances.
- Seasonal Affective Disorder (SAD): This form of depression typically occurs during the winter months when there is less sunlight. Symptoms include fatigue, oversleeping, weight gain, and withdrawal from social activities.
- Postpartum Depression: This condition affects women after childbirth and is marked by feelings of sadness, anxiety , and exhaustion, which interfere with their ability to care for their newborn.
Depression can also be a symptom of other mental health conditions, such as Bipolar Disorder, where periods of depression alternate with episodes of mania. It can also be seen in conditions like Post-Traumatic Stress Disorder (PTSD) or Substance Use Disorders. In these cases, it is essential to distinguish depression from the primary condition to develop an effective treatment plan.
Differentiating Between Depression and Bipolar Disorder
A key difference between Major Depressive Disorder and Bipolar Disorder is the presence of manic episodes in the latter. While individuals with MDD experience only depressive episodes, those with Bipolar Disorder alternate between depression and periods of elevated mood or irritability (mania or hypomania). Accurate diagnosis is crucial for effective treatment, as treatment for Bipolar Disorder may include mood stabilizers or antipsychotics, which differ from treatments for MDD.
Etiology of Depression
The causes of depression are multifaceted, involving a combination of genetic, biological, environmental, and psychological factors:
- Genetic: Individuals with a family history of depression are more likely to develop the disorder.
- Biological: Imbalances in neurotransmitters such as serotonin, dopamine, and norepinephrine are linked to depression.
- Environmental: Life events such as trauma , abuse, or chronic stress can trigger depression.
- Psychological: Negative thinking patterns and low self-esteem can increase the risk of developing depression.
Depression affects various aspects of life, including relationships, work performance, and physical health. Individuals with depression often struggle to maintain social connections, leading to isolation, which can further exacerbate their condition. In relationships , depression can strain communication, intimacy, and emotional support. Additionally, untreated depression may contribute to physical health problems, such as chronic pain or cardiovascular issues, further diminishing the quality of life.
The Importance of Treatment
Early treatment for depression is essential for reducing symptoms and preventing further deterioration. Without treatment, depression can become chronic, leading to impairment in daily functioning and increased risk of suicide. Fortunately, up to 80% of people treated for depression experience improvement in their symptoms within four to six weeks of starting treatment. Unfortunately, nearly two out of three people with depression neither seek nor receive treatment. (Ref)
Treatment Options
- Psychotherapy: Psychotherapy is a cornerstone in treating depressive disorders, offering individuals a safe, supportive space to explore their emotions, thoughts, and behaviors. It is an effective treatment for depression, often providing long-lasting benefits by equipping individuals with coping strategies that last beyond the treatment period. Psychotherapy addresses underlying emotional and behavioral issues that reduce the chances of future depressive episodes while promoting self-awareness, emotional intelligence, and personal growth.
- Medication: Antidepressants, including Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs), are commonly prescribed to balance neurotransmitter levels and alleviate depressive symptoms. In cases of treatment-resistant depression, other medications like mood stabilizers or atypical antipsychotics may be considered.
- Lifestyle Changes: Regular exercise, proper nutrition, and adequate sleep can help improve mood and reduce depressive symptoms. Understanding and addressing life circumstances that exacerbate depression can bring profound relief.
- Electroconvulsive Therapy (ECT): ECT is a treatment option for severe or treatment-resistant depression. It involves brief electrical stimulation of the brain while the patient is under anesthesia and is considered safe and effective for individuals who have not responded to other treatments.
- Support Groups/Group Therapy: Joining a support group allows individuals to connect with others facing similar challenges, providing a sense of community and reducing feelings of isolation.
- Emerging Treatments: Psychedelics and Ketamine: Recent research has shown promise in using psychedelic-assisted therapy and ketamine for the treatment of depression, particularly for treatment-resistant cases. (ref)
Depression can feel isolating, but it's something we can work through together. Whether you're dealing with persistent sadness, lack of motivation, or feeling stuck, we’ll take a close look at what’s contributing to it and find ways to help you feel more like yourself again. We'll build strategies that fit your life and address what’s weighing you down. This is a space where you can be honest about what you're going through, and together, we’ll work on getting you to a place of greater stability and purpose.
